For an appointment about pain, symptoms, risks, and treatment contact us or to learn more about your world renown surgeons at Seattle Neuroscience Institute visit our home page.
Seattle Neuroscience Institute
- Home
- Conditions & Treatments
- Arteriovenous Malformation AVM
- Brain Aneurysm | Cerebral Aneurysm
- Carotid Artery Disease
- Cavernous Malformations
- Colloid Cyst
- Glossopharyngeal Neuralgia
- Hemifacial Spasm
- Meningioma
- Minimally Invasive Spine Surgery
- Moyamoya Disease
- Spinal Canal and Spinal Cord Tumors
- Transient Vertebrobasilar Insufficiency
- Trigeminal Neuralgia
- Research & Publications
- Practice Locations
- About
- Contact
Minimally Invasive Spine Surgery
Cervical and lumbar radiculopathy means nerve root irritation coming from the cervical spine or neck or the lumbar spine or low back. The most common causes of these conditions are disc disease or bone spurs which can irritate the nerves. Disc disease occurs when one or more discs break down or are injured and can press on the nerve roots exiting the lumbar or cervical spine. Lumbar or low back nerve root irritation is often referred to as sciatica, because the sciatic nerve down the back of the leg becomes irritated when the nerve roots exiting the spine, leading to it become compressed. A similar condition can occur in the neck when nerve root irritation produces localized pain in the neck and sometimes pain and weakness in the arm and hand. Most episodes of nerve root irritation in the low back or neck can resolve spontaneously with rest, decreased activity and anti-inflammatory medications. If symptoms become severe and are accompanied by significant weakness, then surgery may be very beneficial for pain relief and to restore function.
Symptoms
Symptoms from cervical radiculopathy
- Severe neck and arm pain
- Arm weakness or clumsiness
- Difficulty using the hand, or severe pain in the hand
Symptoms from lumbar radiculopathy
- Severe back and leg pain
- Pain radiating into the foot
- Leg weakness
- Foot weakness or foot drop( inability to tip the foot back)
Causes
- Herniated or ruptured disc in the neck or low back
- Over growth of ligaments or bone spurs
- Synovial cysts (cysts forming from the lining of the joints)
- Spondylolisthesis or slippage of on joint over the other
- Conditions may occur spontaneously
Risk Factors
- Injury or repetitive use
- Aging process
- Degenerative arthritis, also referred to as osteoarthritis
Diagnosis
The diagnosis of cervical or lumbar radiculopathy is often made on clinical criterion and examination and is usually supplemented by plain x-rays and or MRI of the cervical and lumbar spine. Electrical studies including EMG or electromyography and nerve conduction studies may be used to aid in the diagnosis and differentiate the condition from other nerve problems that are caused by other conditions. Selective nerve root injections may also be used to confirm the diagnosis
Prevention
Prevention of injury and repetitive strain is often effective in preventing clinical episodes of lumbar and cervical raduculopathy
Resources
- Lumbar Degenerative Disk Disease: Background, Pathophysiology, Epidemiology (Medscape)
- Lumbar Degenerative Disc Disease Diagnosis (Spine Health)
- Degenerative Disc Disease Diagnosis | Exams and Tests for DDD (Spine Universe)
- Degenerative Disc Disease – Causes, Symptoms, Risk Factors, Diagnosis (Medtronic)
Treatment
Talk with your doctor about the best treatment plan for you.
Degenerative disc disease is common in aging adults, it seldom requires surgery. When flare ups of pain occur, the majority of patients respond well to non-surgical forms of treatment, and recovery occurs in about six weeks
Non surgical treatment
- Physical therapy, manual therapy
- Medications may be prescribed.
- Anti-inflammatory agents reduce inflammation around the nerve roots while relieving pain.
- Opioid pain relievers may be prescribed short periods for intense pain (acute pain).
Surgical treatment
Surgical treatment may be recommended in patients who fail to respond to initial non surgical treatment or those who develop worsening symptoms, or those who develop new more severe symptoms including weakness and disability.
Minimally invasive surgery
Some patients who require surgery may be candidates for minimally invasive surgical treatment including minimally invasive discectomy or foramenotomy of the cervical or lumbar spine. These procedures most often are done as outpatient procedures and are performed through small tubes which minimize the muscle and ligament damage during the surgical approach and can lead to faster recovery.
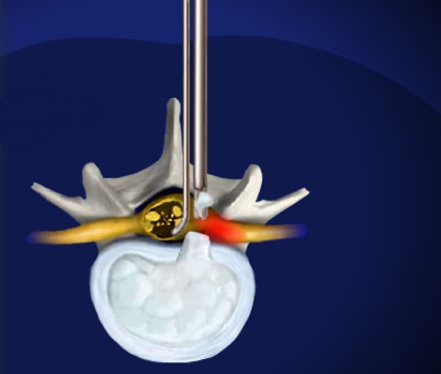
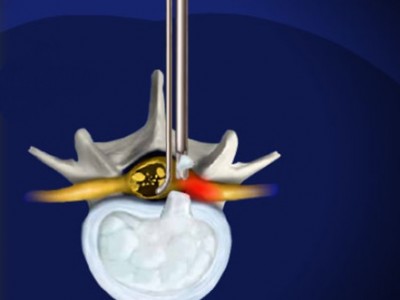
Far Lateral Lumbar Disc Herniation
Lumbar disc rupture or disc herniation is a frequent cause of sciatica or leg pain which originates in the back and radiates down the leg. Symptoms can be quite severe and produce pain, weakness, numbness and difficulty walking. Most disc herniations are within the spinal canal and occur posterior, or directly behind the disc. There is a variant which is called a far lateral lumbar disc and these discs can sometimes be difficult to diagnose and also require a specialized and unique surgical approach to treat. The figure below shows a typical far lateral lumbar disc herniation at the L 4-5 interspace which caused pressure on the L3 nerve root superiorly. The surgical removal for these disc herniations requires a lateral approach rather than a midline approach and can be done through a paramedian incision and can utilize minimally invasive techniques.
Far Lateral approach using minimally invasive metrix technique
The far lateral approach utilizes a small incision made 4.5 centimeters lateral to the midline and insertion of dilators which then allow the insertion of the hollow tube metrix device which allows the surgeon to operate through the tube with specially designed instruments.