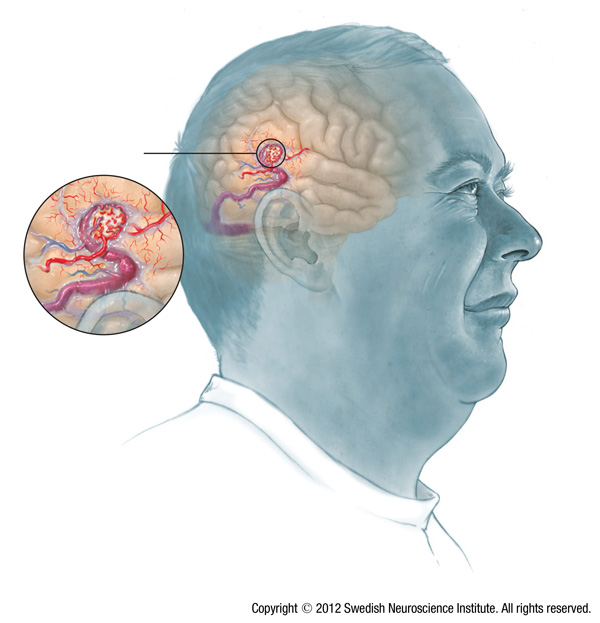
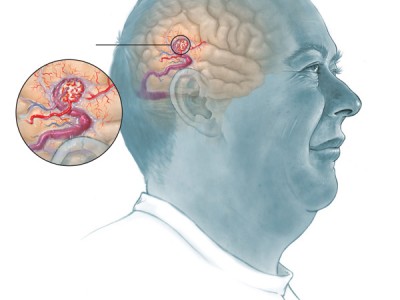
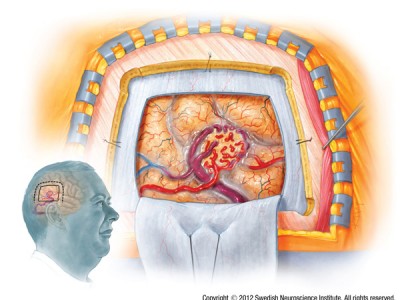
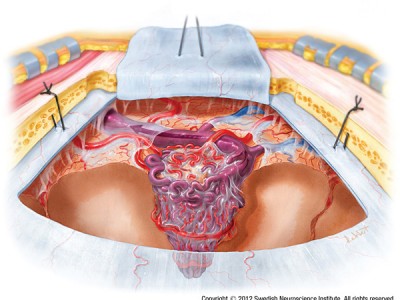
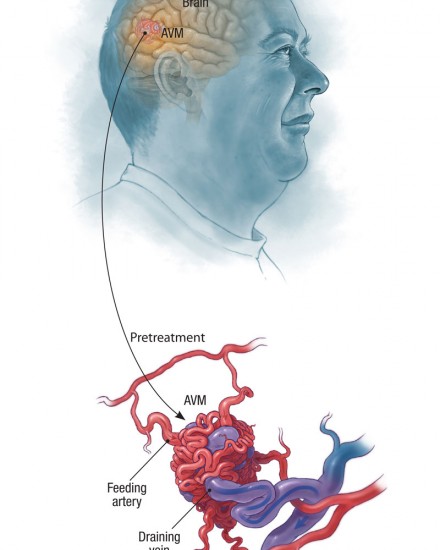
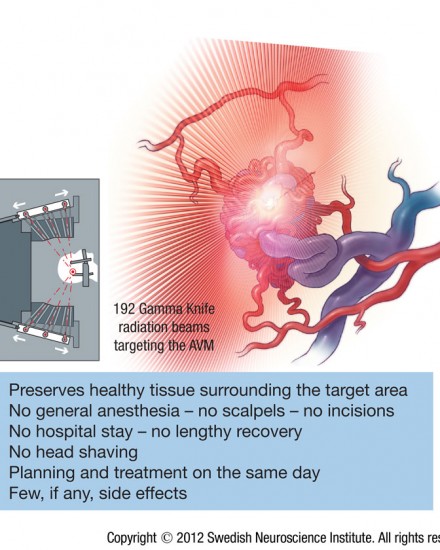
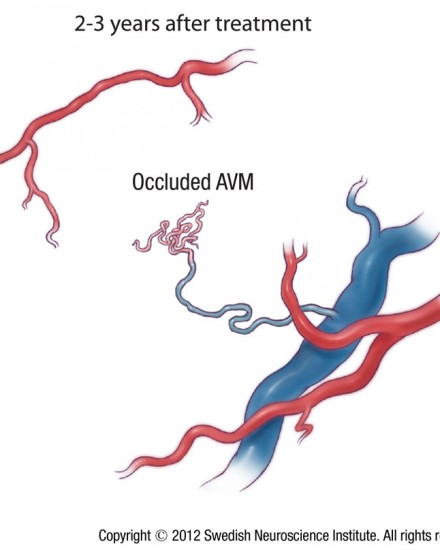
Arteriovenous Malformation AVM. For help with symptoms, risks, and treatment from our world renowned doctors contact us or visit us at Seattle Neurosciences’ website.
Dr. Newell was born in Boston, MA and attended Case Western Reserve University medical school. He then completed his residency in neurosurgery at the University of Washington, including one year in London at St. George’s medical school. Dr. Newell is the co-founder of the Swedish Neuroscience Institute and founder of the Seattle Neuroscience Institute.